The vulva is the part of a woman’s external genital area where the vagina opens. The vaginal lips (inner and outer) are called Labia and the Clitoris is the organ where labial lips meet in the centre.
What is vulvar ulcer?
Vulvar ulcers occur when there are breaks in the skin or mucous membranes of the vulva to expose the underlying tissue. Most of the time vulvar ulcers are painful but occasionally it can be completely asymptomatic. It is usually associated with itching or vaginal discharge.
What are the causes?
Vulvar ulcers may be caused due to local skin problems or may be a part of generalised skin disease. It may be infectious or non-infectious. Genital ulcers are also commonly caused due to sexually transmitted infections like genital herpes, primary syphilis, and vulvo-vaginal candidiasis.
On the other hand, non-sexually transmitted vulvar ulcers can be due to –
- Vulvar or local pathology- The ulceration happens due to vulvar skin problems.
- Systemic illnesses involving vulva – These illnesses affect the whole body along with vulva.
Symptoms
The most common symptoms for vulvar ulcer are itching, pain, soreness or a change in the skin colour and texture of the genital skin. It may be associated with generalised body itch or rashes. They may be painful during intercourse or passage of urine.
Treatment & Prevention
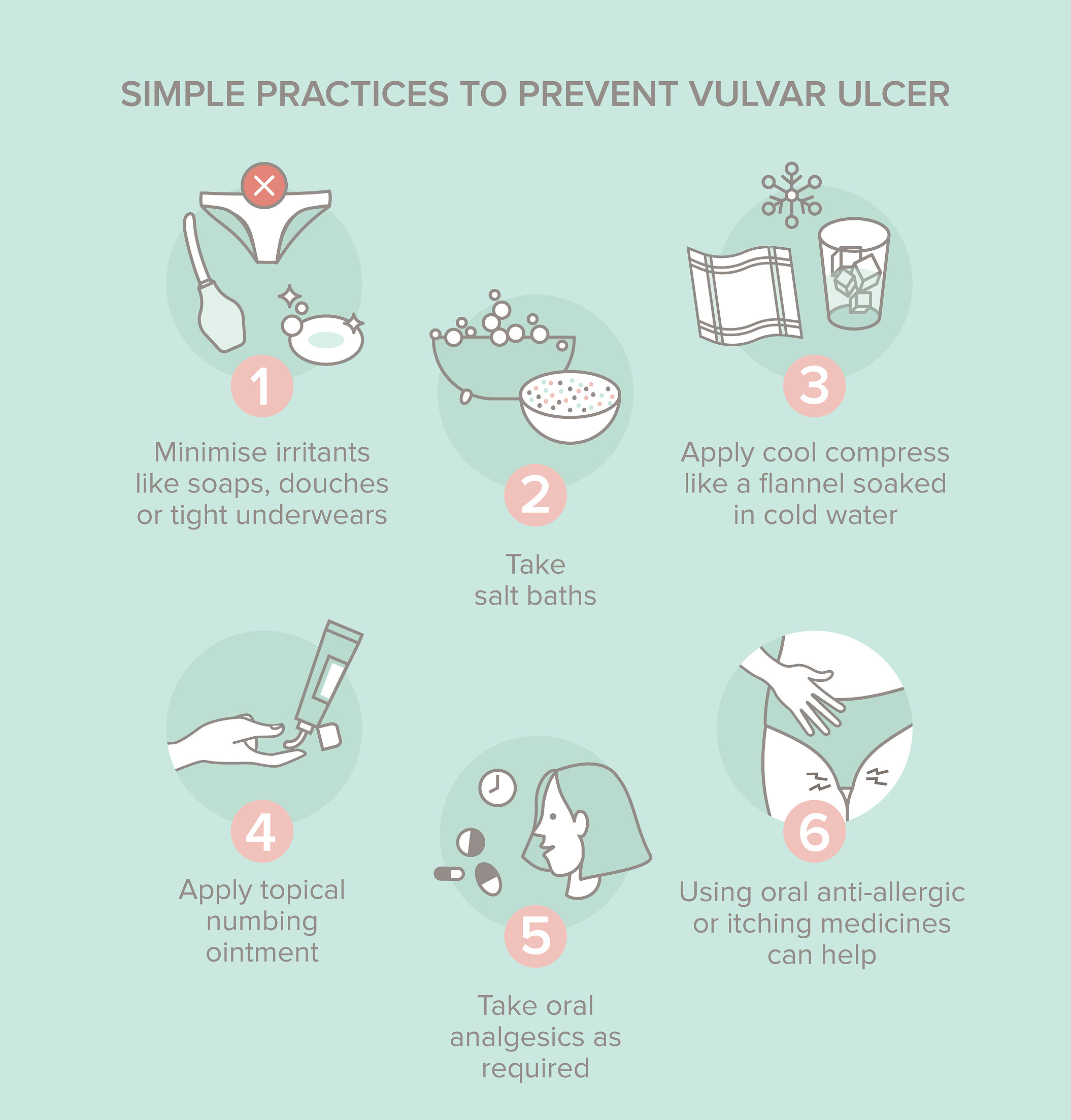
Reassurance and symptomatic treatment addressing the cause is necessary. Non-sexually acquired genital ulcers generally self-resolve without scarring within 2–6 weeks.
In a more serious situation, however, a thorough clinical examination is required to assess the aetiology. If required, the doctor might suggest a biopsy of the ulcer to make a diagnosis. Antiviral medications for herpes infection, local steroid creams or immunosuppressant medications are used to treat systemic illnesses.
Prevention
The skin on the vulva can be very sensitive. Due to heat and humidity, sweating is very common in genital areas. It also makes these areas prone to catch fungal skin infections, itching and dryness.
- Washing or scrubbing with water and soap may increase dryness of the skin and make itching worse. Using gentle lather of the soap while bathing will achieve hygiene. Avoid repeated washings of vulval skin after passing urine. It may be a good habit to dab or pat it dry with tissue.
- Use good moisturiser or aqueous cream application after drying the skin.
- Sanitary towels on a regular basis.
- Wear loose-fitting cotton underwear.
- Avoid tight clothes such as leggings, jeans, and cycling shorts. At home, you may find it more comfortable to wear loose-fitting clothes without underwear.
- Avoid using fabric conditioners and biological washing powders.
- Be careful when using over-the-counter preparations e.g. baby or nappy creams, herbal creams (tea tree oil, aloe vera) and thrush treatments.
- If you tend to scratch your skin, keep your nails trimmed if possible and avoid wearing nail polish.
In short, most vulvar ulcers resolve in 2-6 weeks of correct treatment but if left untreated can have long term serious health implications.
To know more about the intimate parts and how to take care of them, read Dr. Vaishal Joshi’s articles right here. You can also read our expert contents here.









